COMMENTS: A great overview of behavioral addictions. The theme is that substance and behavioral addictions share the same underlying neurological pathways, mechanisms, and behaviors.
Abstract
Background
Several behaviors, besides psychoactive substance ingestion, produce short-term reward that may engender persistent behavior despite knowledge of adverse consequences, i.e., diminished control over the behavior. These disorders have historically been conceptualized in several ways. One view posits these disorders as lying along an impulsive-compulsive spectrum, with some classified as impulse control disorders. An alternate, but not mutually exclusive, conceptualization considers the disorders as non-substance or “behavioral” addictions.
Objectives
Inform the discussion on the relationship between psychoactive substance and behavioral addictions. Methods: We review data illustrating similarities and differences between impulse control disorders or behavioral addictions and substance addictions. This topic is particularly relevant to the optimal classification of these disorders in the forthcoming fifth edition of the American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders.
Results
Growing evidence suggests that behavioral addictions resemble substance addictions in many domains, including natural history, phenomenology, tolerance, comorbidity, overlapping genetic contribution, neurobiological mechanisms, and response to treatment, supporting the DSM-V Task Force proposed new category of Addiction and Related Disorders encompassing both substance use disorders and non-substance addictions. Current data suggest that this combined category may be appropriate for pathological gambling and a few other better studied behavioral addictions, e.g., Internet addiction. There is currently insufficient data to justify any classification of other proposed behavioral addictions.
Conclusions and Scientific Significance
Proper categorization of behavioral addictions or impulse control disorders has substantial implications for the development of improved prevention and treatment strategies.
Introduction
Several behaviors, besides psychoactive substance ingestion, produce short-term reward that may engender persistent behavior despite knowledge of adverse consequences, i.e., diminished control over the behavior. Diminished control is a core defining concept of psychoactive substance dependence or addiction. This similarity has given rise to the concept of non-substance or “behavioral” addictions, i.e., syndromes analogous to substance addiction, but with a behavioral focus other than ingestion of a psychoactive substance. The concept of behavioral addictions has some scientific and clinical heuristic value, but remains controversial. Issues around behavioral addictions are currently being debated in the context of development of DSM-V (1,2)
Several behavioral addictions have been hypothesized as having similarities to substance addictions. The current Diagnostic and Statistical Manual, 4th Edition (DSM-IV-TR) has designated formal diagnostic criteria for several of these disorders (e.g., pathological gambling, kleptomania), classifying them as impulse control disorders, a separate category from substance use disorders. Other behaviors (or impulse control disorders) have been considered for inclusion in the forthcoming DSM – compulsive buying, pathologic skin picking, sexual addiction (non-paraphilic hypersexuality), excessive tanning, computer/video game playing, and internet addiction. Which behaviors to include as behavioral addictions is still open for debate (3). Not all impulse control disorders, or disorders characterized by impulsivity, should be considered behavioral addictions. Although many of the impulse control disorders (e.g., pathological gambling, kleptomania) appear to share core features with substance addictions, others, such as intermittent explosive disorder, may not. In the hope of contributing to this debate, this paper reviews the evidence for similarities between behavioral addictions and substance use disorders, their distinction from obsessive compulsive disorder, and identifies areas of uncertainty warranting future research. It also serves as an introduction to the succeeding papers in this issue, which review some putative addictive behaviors in more detail.
Common Features of Behavioral Addictions: Relationship to Substance Use Disorders
The essential feature of behavioral addictions is the failure to resist an impulse, drive, or temptation to perform an act that is harmful to the person or to others (4). Each behavioral addiction is characterized by a recurrent pattern of behavior that has this essential feature within a specific domain. The repetitive engagement in these behaviors ultimately interferes with functioning in other domains. In this respect, the behavioral addictions resemble substance use disorders. Individuals with substance addictions report difficulties in resisting the urge to drink or use drugs.
Behavioral and substance addictions have many similarities in natural history, phenomenology, and adverse consequences. Both have onset in adolescence and young adulthood and higher rates in these age groups than among older adults (5). Both have natural histories that may exhibit chronic, relapsing patterns, but with many people recovering on their own without formal treatment (so-called “spontaneous” quitting) (6).
Behavioral addictions are often preceded by feelings of “tension or arousal before committing the act” and “pleasure, gratification or relief at the time of committing the act” (4). The ego-syntonic nature of these behaviors is experientially similar to the experience of substance use behaviors. This contrasts with the ego-dystonic nature of obsessive-compulsive disorder. However, both behavioral and substance addictions may become less ego-syntonic and more ego-dystonic over time, as the behavior (including substance taking) itself becomes less pleasurable and more of a habit or compulsion (2,7), or becomes motivated less by positive reinforcement and more by negative reinforcement (e.g., relief of dysphoria or withdrawal).
Behavioral and substance addictions have phenomenological similarities. Many people with behavioral addictions report an urge or craving state prior to initiating the behavior, as do individuals with substance use disorders prior to substance use. Additionally, these behaviors often decrease anxiety and result in a positive mood state or “high”, similar to substance intoxication. Emotional dysregulation may contribute to cravings in both behavioral and substance use disorders (8). Many people with pathological gambling, kleptomania, compulsive sexual behavior, and compulsive buying report a decrease in these positive mood effects with repeated behaviors or a need to increase the intensity of behavior to achieve the same mood effect, analogous to tolerance (9–11). Many people with these behavioral addictions also report a dysphoric state while abstaining from the behaviors, analogous to withdrawal. However, unlike substance withdrawal, there are no reports of physiological prominent or medically serious withdrawal states from behavioral addictions.
Pathological gambling, the most thoroughly studied of the behavioral addictions, provides further insight into the relationship of behavioral addictions and substance use disorders (see also Wareham and Potenza, this issue). Pathological gambling usually begins in childhood or adolescence, with males tending to start at an earlier age (5,12), mirroring the pattern of substance use disorders. Higher rates of pathological gambling are observed in men, with a telescoping phenomenon observed in females (i.e., women have a later initial engagement in the addictive behavior, but foreshortened time period from initial engagement to addiction) (13). The telescoping phenomenon has been extensively documented in a variety of substance use disorders (14).
As in substance use disorders, financial and marital problems are common in behavioral addictions. Individuals with behavioral addictions, like those with substance addictions, will frequently commit illegal acts, such as theft, embezzlement, and writing bad checks, to either fund their addictive behavior or cope with the consequences of the behavior (15).
Personality
Individuals with behavioral addictions and those with substance use disorders both score high on self-report measures of impulsivity and sensation-seeking and generally low on measures of harm avoidance (16–20). However, individuals with some behavioral addictions, such as internet addiction or pathological gambling, may also report high levels of harm avoidance (21; see also Weinstein and Lejoyeux, this issue). Other research has suggested that aspects of psychoticism, interpersonal conflict, and self-directedness may all play a role in internet addiction (see Weinstein and Lejoyeux, this issue). In contrast, individuals with obsessive compulsive disorder generally score high on measures of harm avoidance and low on impulsivity (17,21). Individuals with behavioral addictions also score high on measures of compulsivity, but these may be limited to impaired control over mental activities and worries about losing control over motor behaviors (22). Impaired inhibition of motor responses (impulsivity) has been found in individuals with obsessive compulsive disorder and pathologic skin picking (a behavioral addiction with arguably closer phenomenological links to obsessive compulsive disorder), whereas cognitive inflexibility (thought to contribute to compulsivity) was limited to obsessive compulsivity disorder (23,24).
Comorbidity
Although most nationally representative studies have not included assessment of behavioral addictions, existing epidemiological data support a relationship between pathological gambling and substance use disorders, with high rates of co-occurrence in each direction (25,26). The St. Louis Epidemiologic Catchment Area (ECA) study found high rates of co-occurrence for substance use disorders (including nicotine dependence) and pathological gambling, with the highest odds ratios generally observed between gambling, alcohol use disorders, and antisocial personality disorder (25). A Canadian epidemiological survey estimated that the relative risk for an alcohol use disorder increased 3.8-fold when disordered gambling was present (27). Among individuals with substance dependence, the risk of moderate to high severity gambling was 2.9 times higher (28). Odds ratios ranging from 3.3 to 23.1 have been reported between pathological gambling and alcohol use disorders in U.S. population-based studies (25; 29). Internet addiction was associated with harmful alcohol use (odds ratio of 1.84) in a study of 2,453 college students, after controlling for gender, age and depression (30).
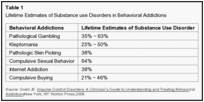
Clinical samples of other behavioral addictions suggest that co-occurrence with substance use disorders is common (Table 1). These findings suggest that behavioral addictions may share a common pathophysiology with substance use disorders.
However, data about substance use comorbidity must be interpreted cautiously because any causal associations may manifest on a behavioral level (for example, alcohol use disinhibits a range of inappropriate behaviors, including those identified as addictive) or on a syndromal level (for example, a behavioral addiction starts after alcoholism treatment, possibly as a substitute for drinking). Problem gamblers with frequent alcohol use have greater gambling severity and more psychosocial problems resulting from gambling than those without alcohol use histories (31), and adolescents who are moderate to high frequency drinkers are more likely to gamble frequently than those who are not (32), suggesting a behavioral interaction between alcohol and gambling. In contrast, a similar finding regarding nicotine use suggests a syndromal interaction, as does the fact that adults with pathological gambling who are current or prior smokers had significantly stronger urges to gamble (33). Problem gamblers who use tobacco daily are more likely to have alcohol and drug use problems (34).
Other psychiatric disorders, such as major depressive disorder, bipolar disorder, obsessive compulsive disorder, and attention deficit hyperactivity disorder, are also commonly reported in association with behavioral addictions (35,36; see also Weinstein and Lejoyeux, this issue). However, many of these comorbidity studies were based on clinical samples. The extent to which these findings generalize to community samples remains to be determined.
Neurocognition
Behavioral addictions and substance use disorders may have common cognitive features. Both pathological gamblers and individuals with substance use disorders typically discount rewards rapidly (37) and perform disadvantageously on decision-making tasks (38) such as the Iowa Gambling Task, a paradigm that assesses risk-reward decision making (39). In contrast, a study of individuals with internet addiction demonstrated no such deficits in decision-making on the Iowa Gambling Task (40). A study using a comprehensive neurocognitive battery in 49 pathological gamblers, 48 abstinent alcohol-dependent subjects, and 49 controls found that gamblers and alcoholics both showed diminished performance on tests of inhibition, cognitive flexibility, and planning tasks, but had no differences on tests of executive functioning (41).
Common Neurobiological Processes
A growing body of literature implicates multiple neurotransmitter systems (e.g., serotonergic, dopaminergic, noradrenergic, opioidergic) in the pathophysiology of behavioral addictions and substance use disorders (42). In particular, serotonin (5-HT), which is involved with inhibition of behavior,, and dopamine, involved with learning, motivation, and the salience of stimuli, including rewards,, may contribute significantly to both sets of disorders (42,43).
Evidence for serotonergic involvement in behavioral addictions and substance use disorders comes in part from studies of platelet monoamine oxidase B (MAO-B) activity, which correlates with cerebrospinal fluid (CSF) levels of 5-hydroxyindole acetic acid (5-HIAA, a metabolite of 5-HT) and is considered a peripheral marker of 5-HT function. Low CSF 5-HIAA levels correlate with high levels of impulsivity and sensation-seeking and have been found in pathological gambling and substance use disorders (44). Pharmacologic challenge studies that measure hormonal response after administration of serotonergic drugs also provide evidence for serotonergic dysfunction in both behavioral addictions and substance use disorders (45).
The repetitive use of substances or engagement in a behavioral addiction following an urge may reflect a unitary process. Preclinical and clinical studies suggest that an underlying biological mechanism for urge-driven disorders may involve the processing of incoming reward input by the ventral tegmental area/nucleus accumbens/orbital frontal cortex circuit (46,47). The ventral tegmental area contains neurons that release dopamine to the nucleus accumbens and orbital frontal cortex. Alterations in dopaminergic pathways have been proposed as underlying the seeking of rewards (gambling, drugs) that trigger the release of dopamine and produce feelings of pleasure (48).
Limited evidence from neuroimaging studies supports a shared neurocircuitry of behavioral addictions and substance use disorders (7). Diminished activity of the ventral medial prefrontal cortex (vmPFC) has been associated with impulsive decision making in risk-reward assessments and with decreased response to gambling cues in pathological gamblers (49). Similarly abnormal vmPFC functioning has been found in people with substance use disorders (50). Game cue-associated brain activation in Internet gaming addicts occurs in the same brain regions (orbitofrontal, dorsolateral prefrontal, anterior cingulate, nucleus accumbens) as with drug cue-associated brain activation in drug addicts (51; see also Weinstein and Lejoyeux, this issue).
Brain imaging research suggests that the dopaminergic mesolimbic pathway from the ventral tegmental area to the nucleus accumbens may be involved in both substance use disorders and pathological gambling. Subjects with pathological gambling demonstrated less ventral striatal neuronal activity with fMRI while performing simulated gambling than did control subjects (52), similar to observations in alcohol-dependent subjects when processing monetary rewards (53). Diminished ventral striatal activation has also been implicated in the cravings associated with substance and behavioral addictions (41). Participation in a gambling task appears to elicit greater dopamine release in the ventral striatum in individuals with Parkinson’s disease (PD) and pathological gambling than in individuals with PD alone (54), a response similar to that elicited by drug or drug-associated cues in drug addicts (55).
Dopamine involvement in behavioral addictions is also suggested by studies of medicated PD patients (56,57). Two studies of patients with PD found that more than 6% experienced a new onset behavioral addiction or impulse control disorder (e.g., pathological gambling, sexual addiction), with substantially higher rates among those taking dopamine agonist medication (58,59). A higher levo-dopa dose equivalence was associated with greater likelihood of having a behavioral addiction (59). Contrary to what might be expected from dopamine involvement, antagonists at dopamine D2/D3 receptors enhance gambling-related motivations and behaviors in non-PD individuals with pathological gambling (60) and have no efficacy in the treatment of pathological gambling (61,62). Further research is warranted to clarify the precise role of dopamine in pathological gambling and other behavioral addictions.
Family History and Genetics
Relatively few family history/genetics studies of behavioral addiction have been designed with appropriate control groups (7). Small family studies of probands with pathological gambling (63), kleptomania (64), or compulsive buying (65) each found that first-degree relatives of the probands had significantly higher lifetime rates of alcohol and other substance use disorders, and of depression and other psychiatric disorders, than did control subjects. These controlled family studies support the view that behavioral addictions may have a genetic relationship to substance use disorders.
The genetic versus environmental contributions to specific behaviors and disorders can be estimated by comparing their concordance in identical (monozygotic) and fraternal (dizygotic) twin pairs. In a study of male twins using the Vietnam Era Twin Registry, 12% to 20% of the genetic variation in risk for pathological gambling and 3% to 8% of the nonshared environmental variation in risk for pathological gambling was accounted for by risk for alcohol use disorders (66). Two-thirds (64%) of the co-occurrence between pathological gambling and alcohol use disorders was attributable to genes that influence both disorders, suggesting overlap in the genetically transmitted underpinnings of both conditions. These findings are similar to those suggesting common genetic contributions to a range of substance use disorders (67).
There are very few molecular genetic studies of behavioral addictions. The D2A1 allele of the D2 dopamine receptor gene (DRD2) increases in frequency from individuals with non-problematic gambling to pathological gambling and co-occurring pathological gambling and substance use disorders (68). Several DRD2 gene single nucleotide polymorphisms (SNPs) have been associated with personality measures of impulsivity and experimental measures of behavioral inhibition in healthy volunteers (69), but these have not been evaluated in people with behavioral addictions. Excessive internet users had higher frequencies of the long-arm allele (SS) of the serotonin transporter gene (5HTTLPR) than healthy controls, and this was associated with greater harm avoidance (70; see also Weinstein and Lejoyeux, this issue).
Responsiveness to Treatment
Behavioral addictions and substance use disorders often respond positively to the same treatments, both psychosocial and pharmacological. The 12-step self-help approaches, motivational enhancement, and cognitive behavioral therapies commonly used to treat substance use disorders have been successfully used to treat pathological gambling, compulsive sexual behavior, kleptomania, pathologic skin picking, and compulsive buying (71–74). Psychosocial interventions for both behavioral addictions and substance use disorders often rely on a relapse prevention model that encourages abstinence by identifying patterns of abuse, avoiding or coping with high risk situations, and making lifestyle changes that reinforce healthier behaviors. In contrast, successful psychosocial treatments for obsessive-compulsive disorder emphasize exposure and response prevention strategies (2).
There are no medications currently approved for the treatment of behavioral addictions, but some medications that have shown promise in treating substance use disorders have also shown promise in treating behavioral addictions (75). Naltrexone, a mu-opioid receptor antagonist approved by the US Food and Drug Administration for the treatment of alcoholism and opioid dependence, has shown efficacy in controlled clinical trials for the treatment of pathological gambling and kleptomania (76–79), and promise in uncontrolled studies of compulsive buying (80), compulsive sexual behavior (81), internet addiction (82), and pathologic skin picking (83). These findings suggest that mu-opioid receptors play a similar role in behavioral addictions as they do in substance use disorders, possibly through modulation of the dopaminergic mesolimbic pathway. In contrast, the short-acting mu-opioid receptor antagonist naloxone exacerbates symptoms in obsessive-compulsive disorder (84).
Medications that alter glutamatergic activity have also been used to treat both behavioral addictions and substance dependence. Topiramate, an anti-convulsant which blocks the AMPA subtype of glutamate receptor (among other actions), has shown promise in open-label studies of pathological gambling, compulsive buying, and compulsive skin picking (85), as well as efficacy in reducing alcohol (86), cigarette (87), and cocaine (88) use. N-acetyl cysteine, an amino acid that restores extracellular glutamate concentration in the nucleus accumbens, reduced gambling urges and behavior in one study of pathological gamblers (89), and reduces cocaine craving (90) and cocaine use (91) in cocaine addicts. These studies suggest that glutamatergic modulation of dopaminergic tone in the nucleus accumbens may be a mechanism common to behavioral addiction and substance use disorders (92).
Diagnostic Issues
Only one behavioral addiction, pathological gambling, is a recognized diagnosis in DSM-IV and ICD-10. Its diagnostic criteria are conceptually similar to those for substance abuse/dependence, i.e., preoccupation with the behavior, diminished ability to control the behavior, tolerance, withdrawal, and adverse psychosocial consequences. The DSM-V Task Force has suggested moving pathological gambling from its current classification as an impulse control disorder to a new classification tentatively termed “Addiction and Related Disorders,” which would include both substance use disorders and “non-substance addictions” (www.dsm5.org, accessed Feb. 10, 2010). The only substantive proposed change in diagnostic criteria is dropping of the criterion regarding commission of illegal acts to finance gambling, which was found to have low prevalence and little effect on the diagnosis.
Several other behavioral addictions have proposed diagnostic criteria, including compulsive buying (93), Internet addiction (94), video/computer game addiction (95), sexual addiction (96), and excessive tanning (see Kouroush et al., this issue). These are usually based on the existing DSM-IV criteria for substance abuse or dependence, e.g., excessive time spent in the behavior, repeated unsuccessful attempts to cut down or stop the behavior, diminished control over the behavior, tolerance, withdrawal, and adverse psychosocial consequences. The DSM-V Substance-Related Disorders work group is considering several of these non-substance addictions for inclusion in DSM-V, specifically mentioning Internet addiction (www.dsm5.org; accessed Feb. 10, 2010). However, for many of the disorders, there are little or no validating data for these diagnostic criteria; they are currently most useful as survey instruments to estimate the prevalence of the problem.
One diagnostic question raised in the literature is where do behavioral addictions (and substance addictions) fall on an impulsivity-compulsivity dimension (97), i.e., are they more like impulse control disorders or obsessive compulsive disorders? Some have argued that this unitary dimension approach is overly simplistic, and that impulsivity and compulsivity represent orthogonal dimensions, rather than opposite poles of a single dimension (98). Consistent with the latter argument are findings such as substantial variation in degree of impulsivity among people with a behavioral addiction, variation that may be associated with response to pharmacological treatment (48, 99).
In DSM-IV, substance addictions (substance use disorders) are an independent category, while pathological gambling is considered an impulse control disorder, similar to, for example, pyromania and kleptomania. ICD-10 classifies pathological gambling as a “habit and impulse” disorder, but recognizes that “the behavior is not compulsive in the technical sense,” even though it is sometimes called “compulsive gambling.”
A related issue is the association, or clustering, if any, among different behavioral addictions. A cluster analysis of demographic and clinical variables in 210 patients with primary obsessive compulsive disorder identified two separate clusters of patients with behavioral addictions (100): patients with pathological gambling or sexual addiction (“hypersexuality”) had earlier age of onset and were more likely male, as compared to patients with compulsive shopping. Further research is needed to confirm and extend this finding. One research approach that might substantially contribute to the field would be a comprehensive evaluation of a large, heterogeneous, well characterized group of individuals with various behavioral and substance addictions in terms of discrete components of impulsivity and compulsivity in both psychological (cognitive) and behavioral (motor) domains, e.g., sensitivity to reward delay (temporal discounting of reward), risk-reward decision-making, conceptual rigidity, premature anticipatory responding, perseverative responding, response inhibition, and reversal learning.
Summary and Conclusions
Growing evidence indicates that behavioral addictions resemble substance addictions in many domains, including natural history (chronic, relapsing course with higher incidence and prevalence in adolescents and young adults), phenomenology (subjective craving, intoxication [“high”], and withdrawal), tolerance, comorbidity, overlapping genetic contribution, neurobiological mechanisms (with roles for brain glutamatergic, opioidergic, serotonergic and dopamine mesolimbic systems), and response to treatment. However, existing data are most extensive for pathological gambling (see Wareham and Potenza, this issue), with only limited data for compulsive buying (see Lejoyeaux and Weinstein, this issue), internet addiction (see Weinstein and Lejoyeaux, this issue), and video/computer game addiction (see Weinstein, this issue), and almost no data for other behavioral addictions such as sexual addiction (see Garcia and Thibaut, this issue), love addiction (see Reynaud, this issue), pathologic skin picking (see Odlaug and Grant, this issue), or excessive tanning (see Kouroush et al., this issue). There is sufficient evidence to warrant considering pathological gambling as a non-substance or behavioral addiction; the DSM-V Task Force has proposed moving its classification in DSM-V from an impulse control disorder to an addiction and related disorders (a new category encompassing both substance-related and non-substance addictions).. In the current state of knowledge, especially in the absence of validated diagnostic criteria and prospective, longitudinal studies, it is still premature to consider other behavioral addictions as full-fledged independent disorders, much less classify them all as similar to substance addictions, rather than as impulse control disorders. Substantial future research, including both human and animal studies (101), is needed to bring our knowledge of behavioral addictions to the level of that for substance addictions, especially in the domains of genetics, neurobiology (including brain imaging), and treatment.
Acknowledgments
Supported by the Intramural Research Program, National Institutes of Health, National Institute on Drug Abuse; NIH (NIDA) grants R01 DA019139 (MNP) and RC1 DA028279 (JEG); and the Minnesota and Yale Centers of Excellence in Gambling Research, which are supported by the National Center for Responsible Gaming and its Institute for Research on Gambling Disorders. Dr. Weinstein is supported by the Israel National Institute for Psychobiology. The contents of the manuscript are solely the responsibility of the authors and do not necessarily represent the official views of the National Center for Responsible Gaming or the Institute for Research on Gambling Disorders or any of the other funding agencies.
Footnotes
Author Disclosures: All authors reported no conflict of interest regarding the content of this paper. Dr. Grant has received research grants from NIMH, NIDA, National Center for Responsible Gaming and its affiliated Institute for Research on Gambling Disorders, and Forest Pharmaceuticals. Dr. Grant receives yearly compensation from Springer Publishing for acting as Editor-in-Chief of the Journal of Gambling Studies, has performed grant reviews for NIH and the Ontario Gambling Association, has received royalties from Oxford University Press, American Psychiatric Publishing, Inc., Norton Press, and McGraw Hill, has received honoraria from Indiana University Medical School, University of South Florida, the Mayo Medical School, the California Society of Addiction Medicine, the State of Arizona, the State of Massachusetts, the State of Oregon, the Province of Nova Scotia, and the Province of Alberta. Dr. Grant has received compensation as a consultant for law offices on issues related to impulse control disorders. Dr. Potenza has received financial support or compensation for the following: consultant for and an advisor to Boehringer Ingelheim; financial interests in Somaxon; research support from the National Institutes of Health, Dept. of Veterans Affairs, Mohegan Sun Casino, National Center for Responsible Gaming and its affiliated Institute for Research on Gambling Disorders, and Forest Laboratories; has participated in surveys, mailings or telephone consultations related to drug addiction, impulse control disorders or other health topics; has consulted for law offices on issues related to addictions or impulse control disorders; has provided clinical care in the Connecticut Department of Mental Health and Addiction Services Problem Gambling Services Program; and has generated books or book chapters for publishers of mental health texts. Dr. Weinstein has received research grants from the Israeli Anti-Drug Authority, the Israel National Institute for Psychobiology, the Chief Scientist of the Israeli Ministry of Health, and the Rashi Trust (Paris, France) and fees for lectures on drug addiction from the Israeli Ministry of Education. Dr. Gorelick reports no outside funding or conflicts of interest.