UPDATES:
- Porn/sex addiction? This page lists 55 neuroscience-based studies (MRI, fMRI, EEG, neuropsychological, hormonal). They provide strong support for the addiction model as their findings mirror the neurological findings reported in substance addiction studies.
- The real experts’ opinions on porn/sex addiction? This list contains 30 recent literature reviews & commentaries by some of the top neuroscientists in the world. All support the addiction model.
- Signs of addiction and escalation to more extreme material? Over 55 studies reporting findings consistent with escalation of porn use (tolerance), habituation to porn, and even withdrawal symptoms (all signs and symptoms associated with addiction).
- An official diagnosis? The world’s most widely used medical diagnostic manual, The International Classification of Diseases (ICD-11), contains a new diagnosis suitable for porn addiction: “Compulsive Sexual Behavior Disorder.”
ARTICLE: Care to weigh in on Internet pornography/cybersex addiction?
Psychiatry’s latest Diagnostic and Statistical Manual (DSM-5) is about to be set in stone. The third and final round of comments ends June 15, 2012. It’s everyone’s duty to take a hard look at this manual. Although many healthcare professionals cheerfully disregard the DSM’s pronouncements when assessing and treating their clients and patients, journalists and insurance companies consider it psychiatry’s bible.
Bizarrely, the DSM-5 has now banished both disorders that address Internet addiction to the appendix—euphemistically renamed “Section III” (items requiring further research). The two disorders are Internet Use Disorder and Hypersexual Disorder (cybersex and pornography excess). This move means these are not officially conditions as far as the doctors of the DSM are concerned.
Yes, you read that correctly. Highspeed Internet is one of the most important phenomena ever to batter the human brain. Dozens of hard-science studies published in the past couple of years reveal that Internet addiction is a physical addiction. Yet those responsible for guiding healthcare professionals in diagnosing addiction disorders have elected to deep-six all relevant bits of the DSM.
Confusingly, the two disorders are not under the purview of the same workgroup, or even found in the same chapter. The titles of both are also somewhat misleading. Internet Use Disorder belies its name, carefully confining itself to Internet gaming rather than encompassing Internet pornography addiction, social media addiction, etc. Prior to banishment, it was in the chapter Substance Use and Addictive Disorders. Hypersexual Disorder, which lists cybersex and pornography, never mentions the word “addiction” at all, leaving any practitioner or journalist relying on the new DSM with the impression that Internet porn addictions can’t exist. It was formerly in the Sexual Dysfunctions chapter.
In short, the DSM’s addiction workgroup is willing to consider (but defer) Internet addiction as long as only “gaming” is mentioned. Why isn’t Internet gaming addiction, with dozens of illuminating research studies defining it, in the manual proper? Why are folks with other Internet addictions (Facebook, compulsive browsing) left out despite a growing number of Internet addiction studies showing addiction-related brain changes?
And why, when those Internet addiction studies generally include porn use, is the Sexual and Gender Identity Disorders workgroup sidestepping the term “addiction?” Is it possible the workgroup is demanding a higher level of proof for Internet porn addiction than was required to legitimize many of the disorders already in the DSM-5’s Sexual Dysfunctions chapter?
Move ’em—don’t lose ’em
What about this idea instead? Move everything related to Internet addictions (gaming, cybersex, social media and pornography) to Substance Use and Addictive Disorders and place it under the jurisdiction of a workgroup of addiction specialists who understand that addiction is fundamentally one condition. In fact, perhaps some physicians from the American Society of Addiction Medicine could help with the task.
Already, gambling addiction has moved to Substance Use and Addictive Disorders. Ideally, all behavioral addictions would be shifted to this chapter and be diagnosed accordingly. At the very least, however, all Internet addictions should be consolidated, relocated, and rescued from the oblivion of Section III.
Although at first glance Internet porn and cybersex addictions may seem like sex addictions, they are, above all, Internet addictions for most sufferers. They arise from the constant novelty afforded by the unique phenomenon of highspeed Internet, which drives overconsumption, leading to addiction-related brain changes. Whether Internet addicts game, chat, browse, or view to excess, their addiction is primarily to novel pixels, even when it’s reinforced with climax.
Internet addiction blind spot is hurting young viewers
If the past is any guide, for the next 15-20 years our society will be saddled with DSM-5, and with journalists and insurance companies blindly relying upon it. Right now, the DSM-5‘s lack of recognition of the risks of Internet porn use is creating a major blind spot in educators, caregivers, users and journalists. Without sound guidance, guys assume that because masturbation is healthy no amount of Internet porn use is unhealthy. Many don’t realize their symptoms are associated with years of continuous highspeed porn use until after they stop.
The fact that adolescent brains are more susceptible to addiction than adult brains makes acknowledgement of Internet addiction in the DSM-5 all the more imperative. Many of today’s young porn users can’t afford to wait until a subsequent DSM finally addresses their addiction-related woes. For some, the situation is dire.
For example, just last week the following articles came out warning of porn-induced sexual dysfunction in young men. (It almost certainly stems from desensitization of the brain’s reward circuitry, an addiction-related change.) All these pieces are either by experts or reporting the observations of experts:
Bottom line: It’s irresponsible to put out a new DSM without proposed diagnostic criteria for Internet addictions. Studies already find rates of Internet addiction ranging from 3% to as high as 25% (in university males).
Sexual politics and historical error
Hypersexual Disorder is the brainchild of the sexologists in the Sexual and Gender Identity Disorders workgroup. Sexologists are perhaps deemed experts on porn use because it can entail masturbation, yet many sexologists also firmly believe that “sex addictions” don’t exist—except perhaps in those with prior mental illnesses. Nor do they acknowledge that Internet porn’s delivery and its users’ habits (e.g., viewing at earlier ages) make it radically different from porn of the past in terms of potential effects on the brain.
As a result, the current DSM-5 imperils addicts. Let’s say you’re mentally healthy and merely addicted to Internet pornography. You are referred to a sexologist adhering to the DSM-5. You face a Hobson’s choice in terms of diagnosis/assessment: Either you have “no problem” and should continue to follow the urgings of your brain’s overtaxed limbic system until you have a disorder, or you have a mental disorder, for which you need psychotropic drugs and counseling. Either way, your healthcare giver does not address your actual affliction: Internet addiction. In contrast, if you had a gambling addiction, you would be diagnosed as an addict under the DSM-5 and offered recovery strategies.
Incidentally, the primary responsibility of the Sexual and Gender Identity Disorders workgroup is to produce guidelines for treating such matters as pedophilia and a variety of colorful fetishes, delayed ejaculation, and kids trying to figure out what gender they are. A quick look at the doctors serving on the Sexual and Gender Identity Disorders workgroup reveals impressive depth in the study of sex offenders, female orgasm, transsexual matters, and so forth, but not one doctor appears to have a strong background in the neuroscience of addiction.
These doctors can spot mental illnesses, but addiction is not on their radar. This blind spot dates back at least 20 years—when an error was made in the field of medicine. When the American Medical Association approved the specialty of addiction medicine, it arbitrarily carved sexual behavior out of the list of possible addictions.
Sex was excluded for political reasons, despite evidence that it should have been incorporated, and an absence of scientific justification for omitting it. (The same circuitry of the brain governs both sex and addictions. All addictions, behavioral and chemical, dysregulate this circuitry—so including sex was virtually a no-brainer.)
At the time, however, Internet porn and cybersex were still in mankind’s future, and genuine sex addicts were few, so the compromise seemed reasonable. Alas, from an addiction-science perspective, it has become increasingly clear that this compromise was an error. With the advent of highspeed Internet, the blunder has come back to bite an entire generation…hard.
Now, we’re facing an untenable situation: The DSM-5‘s sexologists inherited the duty to investigate cybersex and Internet pornography disorders, yet appear to retain a conviction—resting on an historical oversight—that sexual behaviors cannot become addictions (unless the patient has a pre-existing mental illness). Even if their mental-illness paradigm might hold for frotteurs and exhibitionists, there’s no reason to assume it holds for today’s young Internet addicts.
Has the workgroup set the bar for proving the existence of Internet porn addiction too high? What’s the evidence required to validate being a voyeur (a disorder in the manual)? An inability to stop invading others’ privacy despite negative consequences, right? Yet when an Internet porn addict can’t stop despite negative consequences, and decades of brain scans and diagnostic tests combine to explain why, his condition is relegated to the further-research section.
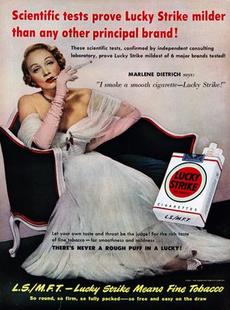
Is asking sexologists to investigate the potentially harmful effects of Internet erotica akin to asking tobacco-company scientists to investigate cigarette addiction?
“Why study unicorns?”
It’s possible the Sexual and Gender Identity Disorders workgroup is still presuming that evidence of addiction, both scientific and otherwise, is largely irrelevant. “Why study unicorns?” asked an academic sexologist when his attention was directed to the severe symptoms and telltale signs of addiction that today’s young Internet addicts are reporting.
Workgroup member Martin P. Kafka, MD devotes less than a page to the possible relevance of addiction neuroscience in his extensive 2009 review Hypersexual Disorder: A Proposed Diagnosis for DSM-V. In Kafka’s defense, much new research elucidating the role of the reward circuitry in both human sexuality and addiction has come out since his review—as well as dozens of studies on Internet addictions of various types. Happily, the DSM-5 still has a year to get up to speed on this important research before releasing the new manual.
The workgroup’s current level of addiction knowledge is evident in the unproductive debate it has been conducting about what might constitute “hypersexual.”
There seems to be deep concern that any suggestion that a behavior facilitating sexual climax can lead to addiction will result in unwarranted scrutiny and labeling of the sexual habits of the promiscuous. Such a fear would be misplaced. The label “addict” does not brand someone as having a moral failing or a mental illness. It means that person needs help changing his behavior he no longer wants in order to reverse some bothersome plastic brain changes.
These are the brain changes that today’s young Internet user must learn to spot long before they mushroom into full-blown addiction. If these signs were public knowledge, many young Internet users could reverse them without ever needing treatment. Why isn’t the DSM-5 encouraging this vital education effort? Why isn’t it addressing how to help Internet addicts change behavior that is distressing them and adversely affecting their sexual performance?
Might the DSM-5 inadvertently be furthering a political agenda that mandates maintenance of the status quo? Certainly, there is no reason for “further study” to continue defining “hypersexuality.” After all, hypersexuality is often not pathological; addiction always is. The decision to move the subjects of cybersex and pornography out of the manual into the former appendix (Section III) effectively keeps the entire matter in limbo, and the focus away from the most promising avenue of analysis: addiction.
This move is especially hard to defend given that the fundamental historical error (which carved “sex” out of the addiction specialty) has now been corrected by the 3000 doctors of the American Society of Addiction Medicine (ASAM). In 2011, ASAM declared addiction a primary illness (no pre-existing mental illness needed), and stated specifically that sexual behavior and food addictions are real, and defined by brain changes, not behaviors. Its public statement is based on decades of neuroscience research.
The DSM’s Sexual and Gender Identity Disorders workgroup members have ignored the addiction specialists of ASAM. As a result, the official voice of the AMA (the DSM-5) does not reflect current addiction science. Ironically, Internet addictions aren’t even sex addictions, as explained above. Internet pornography and cybersex addictions are screen addictions. Take away the screen and the behavior is gone, analogous to video games.
Addiction is one of the most diagnosable disorders
The ultimate irony of locking up all aspects of Internet addiction in the needs-more-study dungeon (Section III), is that the purpose of the original DSM was to improve diagnostic reliability, so mental health professionals could produce a consistent, replicable, scientifically valid results. Rarely in the history of psychiatric medicine has the etiology of any affliction been as well understood as addiction. As diagnostic reliability is the DSM-5‘s mission, it should welcome moving all Internet addictions to Substance Use and Addictive Disorders as a matter of science.
If you’ve read this far, you might appreciate a brief recap of recent addiction neuroscience discoveries: For years, researchers have been able to induce addiction in animal models at will and study their brains in depth. Many of the markers are well understood and some can already be observed and measured in humans.
Next, researchers induced behavioral addictions in animals, using wheel-running and food addiction. (Sorry porn users, scientists can’t induce rats to get it up for pixels, but they can use rats to understand the links between sex and addiction. See below.)
More recently, researchers learned that behavioral addictions (food addiction, pathological gambling, video gaming and Internet addiction) and substance addictions all involve the same fundamental mechanisms, and lead to a collection of shared alterations in brain anatomy and chemistry. (Keep in mind that addictive drugs only cause addiction because they magnify or inhibit mechanisms already in place for natural rewards such as sexual arousal.)
The master switch that triggers many of these addiction-related changes is the protein DeltaFosB. Continued over-consumption of natural rewards (sex, sugar, high-fat, aerobic exercise) or chronic administration of virtually any drug of abuse causes DeltaFosB to accumulate in the reward circuitry. In fact, as hinted at above, researchers have shown that sexual activity causes the accumulation of DeltaFosB, enhancing rats’ “sexual efficiency.”
What other DSM disorder can be reproduced in animal models, or diagnosed with as much reliability as behavioral addiction? Certainly not the many fetish disorders that the Sexual and Gender Identity Disorders workgroup still consider verifiable in the DSM-5: frotteurism, sadomasochism, exhibitionism, transvestism, and so forth. There’s more hard science on behavioral addictions and their assessment (including Internet addiction), and more self-identifying porn addicts complaining of severe consequences.
No need to await further research
The current DSM-5 imposes a harsh sentence on today’s young Internet addicts who don’t have mental illness but need help. The science is solid that behavioral addictions are primary and fundamentally one condition. Gambling addiction is already in the DSM-5; Internet addiction belongs there too. There’s no convincing reason to await further research on Internet addictions.
By consigning Hypersexual Disorder and Internet Use Disorder to oblivion, the current DSM-5 is:
- Disregarding clinical, anecdotal, and experimental evidence that points to Internet addiction as a genuine addiction.
- Ignoring multiple brain studies on Internet addiction disorder, which encompass porn use.
- Encouraging the fiction that the addiction-like signs, symptoms and behaviors reported by Internet porn addicts and their caregivers must necessarily arise from some unidentified mechanisms other than addiction-related brain changes (e.g., “mental illness”).
- Dismissing the addiction-research analysis of medical specialists (ASAM).
- Refusing to acknowledge that Internet erotica is unlike erotica of the past in terms of delivery and the way it is used.
If you have a moment, please encourage the DSM-5 to place all Internet addictions in Substance Use and Addictive Disorders: apa@psych.org
ADDENDUM
The D.S.M. Gets Addiction Right, June 6, 2012
06/07/2012
The D.S.M. Gets Addiction Right – NY Times
By HOWARD MARKEL
Ann Arbor, Mich.
WHEN we say that someone is “addicted” to a behavior like gambling or eating or playing video games, what does that mean? Are such compulsions really akin to dependencies like drug and alcohol addiction — or is that just loose talk?
This question arose recently after the committee writing the latest edition of the Diagnostic and Statistical Manual of Mental Disorders (D.S.M.), the standard reference work for psychiatric illnesses, announced updated definitions of substance abuse and addiction, including a new category of “behavioral addictions.” At the moment, the only disorder featured in this new category is pathological gambling, but the suggestion is that other behavioral disorders will be added in due course. Internet addiction, for instance, was initially considered for inclusion but was relegated to an appendix (as was sex addiction) pending further research.
Skeptics worry that such broad criteria for addiction will pathologize normal (if bad) behavior and lead to overdiagnosis and overtreatment. Allen J. Frances, a professor of psychiatry and behavioral sciences at Duke University who has worked on the D.S.M., has said that the new definitions amount to “the medicalization of everyday behavior” and will create “false epidemics.” Health insurance companies are fretting that the new diagnostic criteria may cost the health care system hundreds of millions of dollars annually, as addiction diagnoses multiply.
There is always potential for misuse when diagnostic criteria are expanded. But on the key scientific point, the D.S.M.’s critics are wrong. As anyone familiar with the history of the diagnosis of addiction can tell you, the D.S.M.’s changes accurately reflect our evolving understanding of what it means to be an addict.
The concept of addiction has been changing and expanding for centuries. Initially, it wasn’t even a medical notion. In ancient Rome, “addiction” referred to a legal dependency: the bond of slavery that lenders imposed upon delinquent debtors. From the second century A.D. well into the 1800s, “addiction” described a disposition toward any number of obsessive behaviors, like excessive reading and writing or slavish devotion to a hobby. The term often implied a weakness of character or a moral failing.
“Addiction” entered the medical lexicon only in the late 19th century, as a result of the over-prescription of opium and morphine by physicians. Here, the concept of addiction came to include the notion of an exogenous substance taken into the body. Starting in the early 20th century, another key factor in diagnosing addiction was the occurrence of physical withdrawal symptoms upon quitting the substance in question.
This definition of addiction was not always carefully applied (it took years for alcohol and nicotine to be classified as addictive, despite their fitting the bill), nor did it turn out to be accurate. Consider marijuana: in the 1980s, when I was training to become a doctor, marijuana was considered not to be addictive because the smoker rarely developed physical symptoms upon stopping. We now know that for some users marijuana can be terribly addictive, but because clearance of the drug from the body’s fat cells takes weeks (instead of hours or days), physical withdrawal rarely occurs, though psychological withdrawal certainly can.
Accordingly, most doctors have accepted changes to the definition of addiction, but many still maintain that only those people who compulsively consume an exogenous substance can be called addicts. Over the past several decades, however, a burgeoning body of scientific evidence has indicated that an exogenous substance is less important to addiction than is the disease process that the substance triggers in the brain — a process that disrupts the brain’s anatomical structure, chemical messaging system and other mechanisms responsible for governing thoughts and actions.
For example, since the early 1990s, the neuropsychologists Kent C. Berridge and Terry E. Robinson at the University of Michigan have studied the neurotransmitter dopamine, which gives rise to feelings of craving. They have found that when you repeatedly take a substance like cocaine, your dopamine system becomes hyper-responsive, making the drug extremely difficult for the addicted brain to ignore. Though the drug itself plays a crucial role in starting this process, the changes in the brain persist long after an addict goes through withdrawal: drug-using cues and memories continue to elicit cravings even in addicts who have abstained for years.
Furthermore, a team of scientists led by Nora Volkow at the National Institute on Drug Abuse have used positron emission tomography (PET) scans to show that even when cocaine addicts merely watch videos of people using cocaine, dopamine levels increase in the part of their brains associated with habit and learning. Dr. Volkow’s group and other scientists have used PET scans and functional magnetic resonance imaging to demonstrate similar dopamine receptor derangements in the brains of drug addicts, compulsive gamblers and overeaters who are markedly obese.
The conclusion to draw here is that though substances like cocaine are very effective at triggering changes in the brain that lead to addictive behavior and urges, they are not the only possible triggers: just about any deeply pleasurable activity — sex, eating, Internet use — has the potential to become addictive and destructive.
Disease definitions change over time because of new scientific evidence. This is what has happened with addiction. We should embrace the new D.S.M. criteria and attack all the substances and behaviors that inspire addiction with effective therapies and support.
Howard Markel, a physician and a professor of the history of medicine at the University of Michigan, is the author of “An Anatomy of Addiction: Sigmund Freud, William Halsted, and the Miracle Drug Cocaine.”
Interesting development that may eventually eclipse DSM and its politics, while providing better care for patients – and above all better understanding of the physiology of mentaldisorders…presumably including behavioral addiction.
05/05/2013
Thomas Insel, director of the NIMH, has recently released this statement pertaining to DSM5: http://www.nimh.nih.gov/about/director/2013/transforming-diagnosis.shtml.
Here is the text:
Transforming Diagnosis
By Thomas Insel on April 29, 2013
In a few weeks, the American Psychiatric Association will release its new edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). This volume will tweak several current diagnostic categories, from autism spectrum disorders to mood disorders. While many of these changes have been contentious, the final product involves mostly modest alterations of the previous edition, based on new insights emerging from research since 1990 when DSM-IV was published. Sometimes this research recommended new categories (e.g., mood dysregulation disorder) or that previous categories could be dropped (e.g., Asperger’s syndrome).1
The goal of this new manual, as with all previous editions, is to provide a common language for describing psychopathology. While DSM has been described as a “Bible” for the field, it is, at best, a dictionary, creating a set of labels and defining each. The strength of each of the editions of DSM has been “reliability” – each edition has ensured that clinicians use the same terms in the same ways. The weakness is its lack of validity. Unlike our definitions of ischemic heart disease, lymphoma, or AIDS, the DSM diagnoses are based on a consensus about clusters of clinical symptoms, not any objective laboratory measure. In the rest of medicine, this would be equivalent to creating diagnostic systems based on the nature of chest pain or the quality of fever. Indeed, symptom-based diagnosis, once common in other areas of medicine, has been largely replaced in the past half century as we have understood that symptoms alone rarely indicate the best choice of treatment.
Patients with mental disorders deserve better. NIMH has launched the Research Domain Criteria (RDoC) project to transform diagnosis by incorporating genetics, imaging, cognitive science, and other levels of information to lay the foundation for a new classification system. Through a series of workshops over the past 18 months, we have tried to define several major categories for a new nosology (see below). This approach began with several assumptions:
- A diagnostic approach based on the biology as well as the symptoms must not be constrained by the current DSM categories,
- Mental disorders are biological disorders involving brain circuits that implicate specific domains of cognition, emotion, or behavior,
- Each level of analysis needs to be understood across a dimension of function,
- Mapping the cognitive, circuit, and genetic aspects of mental disorders will yield new and better targets for treatment.
It became immediately clear that we cannot design a system based on biomarkers or cognitive performance because we lack the data. In this sense, RDoC is a framework for collecting the data needed for a new nosology. But it is critical to realize that we cannot succeed if we use DSM categories as the “gold standard.”2 The diagnostic system has to be based on the emerging research data, not on the current symptom-based categories. Imagine deciding that EKGs were not useful because many patients with chest pain did not have EKG changes. That is what we have been doing for decades when we reject a biomarker because it does not detect a DSM category. We need to begin collecting the genetic, imaging, physiologic, and cognitive data to see how all the data – not just the symptoms – cluster and how these clusters relate to treatment response.
That is why NIMH will be re-orienting its research away from DSM categories. Going forward, we will be supporting research projects that look across current categories – or sub-divide current categories – to begin to develop a better system. What does this mean for applicants? Clinical trials might study all patients in a mood clinic rather than those meeting strict major depressive disorder criteria. Studies of biomarkers for “depression” might begin by looking across many disorders with anhedonia or emotional appraisal bias or psychomotor retardation to understand the circuitry underlying these symptoms. What does this mean for patients? We are committed to new and better treatments, but we feel this will only happen by developing a more precise diagnostic system. The best reason to develop RDoC is to seek better outcomes.
RDoC, for now, is a research framework, not a clinical tool. This is a decade-long project that is just beginning. Many NIMH researchers, already stressed by budget cuts and tough competition for research funding, will not welcome this change. Some will see RDoC as an academic exercise divorced from clinical practice. But patients and families should welcome this change as a first step towards “precision medicine,” the movement that has transformed cancer diagnosis and treatment. RDoC is nothing less than a plan to transform clinical practice by bringing a new generation of research to inform how we diagnose and treat mental disorders. As two eminent psychiatric geneticists recently concluded, “At the end of the 19th century, it was logical to use a simple diagnostic approach that offered reasonable prognostic validity. At the beginning of the 21st century, we must set our sights higher.”3
The major RDoC research domains:
Negative Valence Systems
Positive Valence Systems
Cognitive Systems
Systems for Social Processes
Arousal/Modulatory Systems
References
1Mental health: On the spectrum. Adam D. Nature. 2013 Apr 25;496(7446):416-8. doi: 10.1038/496416a. No abstract available. PMID: 23619674
2Why has it taken so long for biological psychiatry to develop clinical tests and what to do about it? Kapur S, Phillips AG, Insel TR. Mol Psychiatry. 2012 Dec;17(12):1174-9. doi: 10.1038/mp.2012.105. Epub 2012 Aug 7.PMID:22869033
3The Kraepelinian dichotomy – going, going… but still not gone. Craddock N, Owen MJ. Br J Psychiatry. 2010 Feb;196(2):92-5. doi: 10.1192/bjp.bp.109.073429. PMID: 20118450